The Endocannabinoid System and CBD
What is the endocannabinoid system?
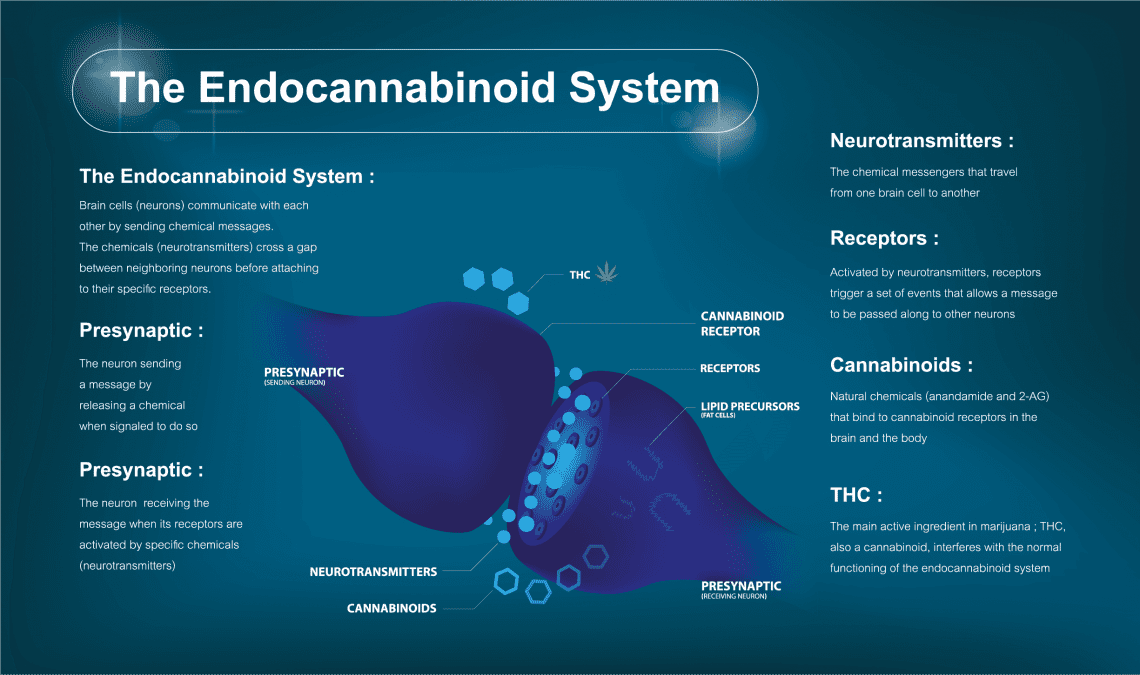
In 1964, researchers in Israel discovered therapeutically active substances in cannabis called cannabinoids and isolated the most popular and possibly effective cannabinoid, THC (tetrahydrocannabinol). More than 20 years later, in 1988, researchers identified the human body’s endocannabinoid system.
Endocannabinoids are the special molecules naturally produced in the human body that are closely related to the proper functioning of the immune system and nervous system and that are mimicked by the cannabinoids found in the cannabis plant. Cannabinoids contained in cannabis, referred to as phytocannabinoids, simply imitate endocannabinoids. Cannabinoids fit perfectly into specialized receptors found throughout the nervous and immune systems, serving to enhance, or improve upon, the body’s own ability to maintain homeostasis (balance) and health.
The role of receptors
Research since the discovery of the endocannabinoid system has led to the identification of specialized receptors in the body. Knowledge of these receptors, called CB1 and CB2, has greatly enhanced the overall knowledge of how cannabinoids synergistically interact with other cannabinoids and endocannabinoids to produce sometimes profound medical effects. An understanding of these receptors also allows for the production of synthetic cannabinoids and specialized extracts that best take advantage of the function of these receptors.
CB1 receptors are located throughout the brain and central nervous system, as well as the kidneys, liver, lungs, digestive tract, and even the eyes. Revealingly, these receptors outnumber those for opiates by a wide margin (possibly as high as 10 to 1). The placement of CB1 receptors is also why overdoses on cannabis are impossible; these receptors are not present in the basal regions of the brain that are responsible for vital functions, such as heart and respiratory function. Overdoses due solely to cannabis use simply do not occur.
CB2 receptors are primarily found in the peripheral organs, in particular tissues associated with the immune system, including the tonsils, thymus, spleen, and bone marrow.
An expert’s explanation
Dr. Ethan Russo, a prominent and well-published cannabinoid researcher, has written a detailed description of the endocannabinoid system and its efficacy for human health:
“The analgesic and palliative effects of cannabis and cannabinoid preparation have been amply reported over the past generation…. In essence, the effects result from a combination of receptor and non-receptor mediated mechanisms. THC and other cannabinoids exert many actions through cannabinoid receptors, G-protein coupled membrane receptors that are extremely densely represented in central, spinal, and peripheral nociceptive pathways.
“Endogenous cannabinoids (endocannabinoids) even regulate integrative pain structures such as the periaqueductal gray matter. The endocannabinoid system also interacts in numerous ways with the endogenous opioid and vanillio systems that can modulate analgesia and with a myriad of other neurotransmitter systems such as the serotonergic, dopaminergic, glutamatergic, etc, pertinent to pain. The current author has suggested that a clinical endocannabinoid deficiency may underlie the pathogenesis of migraine, fibromyalgia, idiopathic bowel syndrome, and numerous other painful conditions that defy modern pathophysiological explanation or adequate treatment.”
Dr. Ethan Russo
– Cannabinoid Researcher
Should Marijuana be Legal for Medicinal Purposes?
Cannabis is medicine
The use of cannabis as medicine dates back nearly 5,000 years. During the 19th century—and up until 1942—cannabis was included in the American pharmacopoeia, a list of effective drugs and how to make them used by doctors and pharmacists at the time. Between 1840 and 1900, more than 100 articles were published in medical journals in the United States regarding the efficacy of cannabis for patients. The period of 1837 to 1937 was called by one historian the “golden age of medical cannabis.”
This growing collection of doctor opinions, anecdotal accounts, and research was cut short with the passage of the Marijuana Tax Act of 1937 in the United States. While the law didn’t specifically outlaw marijuana, it did require a special tax stamp for legal cultivation, possession, and consumption. No such tax stamps were ever granted.
Recent research in countries such as Canada, the United Kingdom, Spain, Israel, and even Mexico has clearly illustrated not only the very promising medical efficacy of the plant, but also the acute need for additional clinical research and human trials. Such studies have shown that cannabis can decrease a patient’s dependence on conventional pharmaceutical treatments and drugs—many of which carry negative side effects that some patients say are, ironically, worse than the conditions for which they are prescribed.
It should be noted that the position of the U.S. government has seemingly shifted over the past couple of years. Beginning in 2013, the federal government began taking certain positions that have led to a greater acceptance of the concept of medical cannabis and the research of cannabis for medical purposes. Many states and many institutions of higher education have taken this opportunity to further evaluate the benefits that cannabis may provide to people in need. In March of 2015, the only federally approved cannabis production facility, located at the University of Mississippi and home to the National Institute for Drug Abuse (NIDA), was given a $69 million grant to produce more cannabis for federally sanctioned medical cannabis research.
Clinical Data
Clinical research regarding the efficacy of cannabis for human health has been severely limited by its CSA scheduling; a Schedule I designation, by definition, means that cannabis has no medical value, and therefore federally sanctioned research with the intent of showing positive efficacy is rarely ever approved. Despite this, some very revealing facts have been learned. Consider, for example, that in excess of 85 cannabinoids have been discovered within the plant, all of which are capable of synergistically interacting with the human endocannabinoid system to produce some response by the human body. Not long ago, NIDA modified a prior statement on medical cannabis to acknowledge that “recent animal studies have shown that marijuana can kill certain cancer cells and reduce the size of others.”
In addition, more than 200 terpenes have been identified in cannabis. These molecules, responsible for the relatively strong aroma of cannabis, function in a very similar manner to cannabinoids and also play a part in the synergistic interaction of marijuana-derived cannabinoids with those produced by the human endocannabinoid system. This is yet another area of the efficacy of cannabis that is largely unknown due to a lack of credible research.
In 1991, the International Cannabinoid Research Society was formed to serve as an organization to study the efficacy of cannabinoids. Similarly, in 2000, the International Association for Cannabis as Medicine was created to encourage and promote clinical research regarding cannabis-based therapy. One year later, the Center for Medical Cannabis Research was established at the University of California San Diego to conduct studies regarding cannabis use as medicine. The group in 2010 published a report that detailed more than one dozen clinical trials it had conducted (many of which were FDA approved). The report concluded that cannabis is an effective treatment in many instances, specifically for the control of pain, and that it works better than many mainstream pharmaceutical drugs and therapies.
Despite the challenges to conducting cannabis research, more than 1,500 peer-reviewed articles about cannabis and its medical efficacy have been published to date. In 2009, a review of clinical studies covering a 38-year period concluded that “Nearly all of the 33 published controlled clinical trials conducted in the United States have shown significant and measurable benefits in subjects receiving…treatment.” This review stated that cannabis is an effective analgesic (pain killer), protects and even improves the nervous system, and is a powerful anti-inflammatory. All of which means that cannabis can effectively treat diseases and symptoms that are poorly or even ineffectively managed by conventional drugs. It can deal with severe pain, help those suffering from neurological disorders like multiple sclerosis, epilepsy, and dystonia, and greatly improve the conditions of cancer and HIV/AIDS patients (including those suffering from other wasting syndromes).
Studies
Despite decades of federal opposition in the U.S., international research into the efficacy of cannabis and cannabinoids has been plentiful. Research organizations in the United Kingdom, Israel, Spain, Italy, and other countries have conducted case studies and clinical investigations into the medical properties of cannabis for a multitude of conditions. These studies have proven the value of both whole-plant cannabis, as well as synthetic and derivative forms of the herb. Despite this, clinical trials involving humans are still grossly lacking, preventing the creation of standardized treatments for particular ailments.
In 1994, the Federation of American Scientists, based on evidence of its superior effectiveness and safety compared to other medications, recommended to the President that the Food and Drug Administration work with the National Institutes of Health to develop protocols to make available cannabis for severely sick patients under the advisement of their physicians. In 1995, the American Public Health Association encouraged robust research on the part of Congress to “move expeditiously to make cannabis available as a legal medicine.”
Since the mid-1990s, numerous professional medical organizations and physician associations, including The American Academy of Family Physicians, have officially supported the use of medical cannabis in the treatment of particular conditions.
A 1999 report from the Institute of Medicine (IOM) entitled Marijuana and Medicine, proclaimed the medical value of cannabis and that further federally authorized research was warranted. The report was the result of two years of analysis conducted by the IOM at the request of the White House Office of National Drug Control Policy. Despite this, the federal approval for follow-up studies was sparse. While some studies have been conducted in the U.S. with animals or cell cultures, almost no human trials have been performed. As detailed in the report, “clinical studies of marijuana are difficult to conduct…there is a daunting thicket of regulations to be negotiated at the federal level.” Researchers and investigators have found it extremely difficult to get federal approval to conduct the studies and, when authorization is provided, it has historically been difficult to obtain quality cannabis samples from the government to conduct the sanctioned research.
The American Nurses Association took a pro-cannabis stance and supported health care providers wanting to recommend cannabis for patients. It declared support for “patients to have safe access to therapeutic cannabis” and called for additional research.
Significant support was provided from the American College of Physicians (ACP) in their position paper of 2008 in which the organization acknowledges that the therapeutic qualities of cannabis are well established and it’s time for studies designed to determine the best dose and route of delivery. The ACP further calls for changes to the Schedule I classification of the plant so badly needed rigorous scientific evaluation can begin immediately.
In response to the ACP’s position paper, Dr. Jocelyn Elders, a former U.S. Surgeon General, marked its significance by stating “large medical associations are by their nature slow and cautious creatures that move only when the evidence is overwhelming,” adding that “[t]he evidence is indeed overwhelming that…there is ‘a clear discord’ between what research tells us and what our laws say about medical marijuana…[i]t’s time to end that ‘clear discord’ and put science ahead of politics.”
These are only a few of the healthcare and research organizations that have supported—and sometimes demanded, in strongly worded articles or proclamations—the legal use of cannabis by sick patients and more robust research involving human trials.
Other groups that have published similar studies, reports, and position papers include the American Public Health Association, the American Preventive Medical Association, the American Academy of Family Physicians, the National Association of Boards of Pharmacy, the American Medical Association, the California Medical Association, the American Society of Addiction Medicine, and the Iowa Board of Pharmacy.
All of these groups echo a common theme: available evidence reveals a strong correlation between cannabis and patient benefit and that the need for additional research is paramount.
For additional relevant medical publications, contact our Community Outreach Coordinator, Christine Karhliker, [email protected].
Cannabis: The Modern Medicine
Cannabis’ impact on the human body can be credited, in large part, to what are called Cannabinoids. Cannabinoids are chemical compounds secreted by the plant’s trichomes that offer a wide array of therapeutic benefits. The two most well known cannabinoids are THC and CBD. Cannabinoids bind to receptor sites in the brain and body – this system of receptors is referred to as the Endocannabinoid System.
The science behind cannabinoids as medicine is strong; so much so that certain cannabinoids have actually been synthesized (artificially made) and received FDA approval for treatment of illnesses like MS (Sativex, Marinol and others). The two cannabinoids mentioned, THC and CBD, have been shown to help patients suffering from pain, nausea, sleep and stress disorders, as well as stress relief, anxiety, inflammation and epilepsy. Cannabis contains at least 85 different cannabinoids and more research becomes available every day detailing how cannabinoids can be used to treat a wide range of ailments. However, recent studies have also shown a possible connection between early cannabis use and a negative impact on brain development. Without question, additional research into cannabis’ impact on the human body is needed and appropriate.
One of the best things to understand about cannabis as a modern medicine is that you no longer have to smoke cannabis or ingest a food/liquid that contains an unknown or random amount of active ingredient. Like traditional modern medicine, cannabis can be precisely dosed. Recent advancements in processing techniques have lead to the ability to have pills, gelcaps, tablets and the like created that contain exact amounts of active ingredient; i.e. 5 mg of THC and 10 mg of CBD — this is a significant advancement in the use of cannabis for medicinal purposes.
THC Dosage: What's the Right Dose for You?
An important aspect of any medical treatment is making sure it’s safe and effective.
Author and pharmacologist Dr. Nichol Iverson explained the dosing testing that has been conducted to date:
“Laboratory animals (rats, mice, dogs and monkeys) can tolerate doses of up to 1000 mg/kg. This would be equivalent to a 70 kg person swallowing 70g of the drug—about 5,000 times more than is required to produce a high. Despite widespread illicit use of cannabis, there are very few, if any, instances of people dying from an overdose.”
In 1988, the Drug Enforcement Administration’s Law Judge, Francis Young—responding to a petition to reschedule cannabis under the Controlled Substances Act (to make it easier to conduct research into its efficacy)—said, “In strict medical terms, marijuana is far safer than many foods we commonly consume…. Marijuana, in its natural form, is one of the safest therapeutically active substances known to man. By any measure of rational analysis, marijuana can be safely used within the supervised routine of medical care.”
The Institute of Medicine (IOM), more than 10 years later, when investigating the physiological risks of cannabis use, concluded that “Marijuana is not a completely benign substance. It is a powerful drug with a variety of effects. However, except for the harms associated with smoking, the adverse effects of marijuana use are within the range of effects tolerated for other medications.”
Research conducted on the long-term effects of cannabis use since the IOM report has revealed that consumption of moderate amounts of cannabis to be remarkably safe, particularly when compared to other therapeutically active substances — most significantly is the relative lack of overdose risk. According to a 1995 review prepared for the World Health Organization, “there are no recorded cases of overdose fatalities attributed to cannabis”. Furthermore, a review of clinical investigations and observational studies detailed that investigators “did not find a higher incidence rate of serious adverse events associated with medical cannabinoid use.”
Toxicity and overdose risk
It is estimated that to overdose, an average sized human would need to consume 1,500 pounds of cannabis in 15 minutes—an act that is truly not possible. Using a system called LD50, which indicates the lethal dose of a drug or substance for 50 percent of the population, researchers have determined that cannabis is one of the safest substances known and one from which it is theoretically impossible to overdose. Dr. Lester Grinspoon, a psychiatry professor at Harvard Medical School, wrote the following in 1995 in the Journal of the American Medical Association:
“One of marihuana’s greatest advantages as a medicine is its remarkable safety. It has little effect on major physiological functions. There is no known case of a lethal overdose; on the basis of animal models, the ratio of lethal to effective dose is estimated as 40,000 to 1. By comparison, the ratio is between 3 and 50 to 1 for secobarbital and between 4 and 10 to 1 for ethanol [alcohol].”
“Marihuana is also far less addictive and far less subject to abuse than many drugs now used as muscle relaxants, hypnotics, and analgesics. The chief legitimate concern is the effect of smoking on the lungs. Cannabis smoke carries even more tars and other particulate matter than tobacco smoke. But the amount smoked is much less, especially in medical use, and once marihuana is an openly recognized medicine, solutions may be found; ultimately, a technology for the inhalation of cannabinoid vapors could be developed.”
The technology to which Dr. Grinspoon alluded is now available via desktop and pocket vaporizers from dozens of manufacturers. Because research regarding the rate of lung cancer and pulmonary diseases, even among chronic cannabis consumers, has shown that marijuana smokers experience no greater risk of lung cancer or related diseases. In fact, research has demonstrated that heavy cannabis smokers are at no greater risk of lung cancer than non-smokers.
Despite these findings, cannabis can’t be considered “harmless.” It delivers a variety of physiological effects, including dilation of blood vessels and rapid heart rate. In very limited cases, especially among those with cardiac conditions, these symptoms can be dangerous. However, these adverse effects are well within the range of other FDA-approved medications. Also, because of tolerance building, users often overcome such reactions to the herb.
Dr. Grinspoon added:
“The greatest danger in medical use of marihuana is its illegality, which imposes much anxiety and expense on suffering people, forces them to bargain with illicit drug dealers, and exposes them to the threat of criminal prosecution.”
What Are the Different Ways to Consume Marijuana?
These days, a wide variety of consumption methods exist. Traditionally, cannabis is smoked in either a pipe-type instrument or rolled in paper and smoked like a cigarette (a joint). Oral ingestion (eating cannabis-infused foods) has also been a traditional consumption method in many cultures.
Recently, with advancements in extraction technologies, a new form of concentrated resin has been developed as well as concentrated forms of cannabis oils that can be ingested orally, mixed with topical lotions and applied to the skin, or vaporized and inhaled – smoking the flower is no longer the only method; you can truly take a pill that contains a very precise and consistent dosage of medication, i.e. a pill with 5mg of THC and 5mg of CBD.
There’s a method for everyone
While the medical efficacy of cannabis is undeniable, it is important to use the delivery system that is the best fit for you and your condition. Each consumption method produces different effects at different durations. Therefore, certain methods of consumption will be better than others in the treatment of each condition.
Here is a quick rundown of the most common forms of consumption and the cannabis forms for each:
- Inhalation – smoking or vaporizing and inhaling through the lungs (joints, pipes, and vaporizers).
- Ingestion – the cannabinoids and terpenes are extracted from the flower as oil and then either ingested as-is, combined with another medium like food or processed into pills, gel caps and other traditionally seen medicinal forms that can enable very precise and controlled dosing experiences (edible baked goods, pills, capsules and tinctures).
- Oral absorption – the extracted oil is combined with another medium. The finished product is kept in the mouth while it dissolves under the tongue, on the tongue or through the inner cheek (mints, lozenges and breath strips).
- Topical – the extracted oil is combined with a product that is applied to the skin (lotion, ointments and transdermal patches).
- Cannabis suppositories.
Inhalation
There are two different methods of inhalation — smoking and vaporizing —both of which provide a rapid onset and similar effects. While both involve heating cannabis so that cannabinoids are absorbed directly into the bloodstream through the lungs, they are two very different methods. Smoking cannabis involves lighting dried cannabis flowers with fire in a method known as combustion – this includes using pipes, and joints.
The healthier delivery system, vaporizing, uses a stream of heated air to vaporize the active ingredients in cannabis without combustion. Unlike smoking, both cannabis concentrates and dried flowers can be vaporized.
Ingestion
Ingesting cannabis produces much stronger and more psychoactive effects than other delivery systems. When digested, cannabinoids are broken down in the gastrointestinal tract and then passed through the liver before entering the bloodstream. As a result of this process, the cannabinoids pass through the blood-brain barrier more effectively, thereby increasing potency by making them more likely to bind with the endocannabinoid receptors throughout the body. It may take 30 minutes to 2 hours to feel the full effects from ingested cannabis.
Edible cannabis effects everyone a little bit differently, depending on body size, metabolism, and experience. Many people associate edible cannabis with the traditional ‘pot brownie,’ but that hardly gives this method the credit it deserves. Truly medicinal cannabis is grounded in edible applications of cannabis — like most traditional medical applications, specific cannabinoids can now be reduced to pill form, capsules, tablets and liquid form. These new forms allow for very controlled and repeatable dosing events — like traditional pharmaceutical medicines, you can now take a pill that contains precisely 5 mg of THC or CBD and so on.
A closer look at edibles
The most important thing to remember is that each person can be different – start low and go slow. The metabolism of the person plays a large role in the amount of time it takes for an edible to take effect. Traditionally, it can take anywhere from 20 minutes to two hours or longer.
The effects generally peak up to four hours after eating or drinking cannabis, so it’s best to wait at least that long before consuming more. In most places, 5-10mg is considered to be a dose – which may be just right for some, too much or not enough for others. Take your time and learn what’s right for you, and always pay attention to the label for dosing and recommended serving size.
Oral absorption
Cannabinoids can be absorbed directly into the bloodstream from 3 different areas inside the mouth — under the tongue (sublingual), on the tongue, and all other mucosa tissues lining inside the entire mouth.
The full effects from using this delivery system will be felt more quickly than by ingesting, but less quickly than with inhalation. The cannabinoids will be absorbed most quickly when held under the tongue. Most commonly, cannabis is consumer orally with infused mints, lozenges, and breath strips. In this method of delivery, the effects will be felt within 10 to 60 minutes.
Topicals
Topical medical cannabis products come in a variety of forms including lotions, balms, creams, salves and patches. Topical medical marijuana products are applied to the outside of the skin, and can provide localized relief from inflammation, pain, skin irritations and more.
In all forms of topical application other than patches, cannabinoids react with receptors under the skin, but they do not reach the bloodstream. As a result, most topical medical cannabis products do not provide psychoactive effects. Some transdermal patches, however, are able to transfer cannabinoids into the bloodstream.
Cannabis suppositories: what are they and how do they work?
A suppository is an ovular capsule that’s meant to be inserted vaginally or rectally. In the case of rectal cannabis suppositories, the capsules are typically about an inch long and are made from a mixture of coconut oil infused with cannabis or FECO (Full Extract Cannabis Oil)-infused cocoa butter.
Once inserted, the capsule dissolves and is absorbed into the bloodstream through the thin lining of the intestinal wall. Unlike some other forms of medical cannabis, rectal cannabis suppositories are incredibly bioavailable – meaning they’re easy for the body to use.
Rectal cannabis suppositories have an efficiency rate of between 50-70 percent and produce predictable effects every time they are used. Additionally, rectal cannabis suppositories take only 10-15 minutes to take effect and the medical effects can last for between four and eight hours.
Are you a candidate for rectal cannabis?
Chemotherapy patients experiencing extreme nausea who can’t stomach edible marijuana but need pain relief nonetheless.
Another example is elderly patients who can’t swallow pills or patients headed into surgery who are not allowed to ingest anything orally in the hours before their procedure. These patients would all be good candidates for rectal cannabis. Patients who simply don’t like the effects of edible or inhaled marijuana may prefer cannabis suppositories, as well.
What are the effects of cannabis suppositories?
Once a cannabis suppository has been administered, you’ll begin to feel the effects quite quickly. Generally, this begins as a warm, liquid feeling that starts in the pelvis and spreads throughout the rest of the body. If you’ve been experiencing pain or anxiety, the symptoms will likely begin to subside immediately.
Unlike other forms of medical cannabis, rectal suppositories don’t make users “high,” so you’ll still feel clear-minded and sharp. The effects of rectal cannabis can last for up to eight hours without re-administration.
Information obtained from hellomd.com





